

Introduction to Health as a Core American Value
Health has long been a pivotal aspect of American culture, tracing its roots back to the early days of the American colonies. The focus on health was significantly shaped by the practices and beliefs of Native American tribes, who possessed extensive knowledge of medicinal plants and holistic healing techniques. European settlers, upon arriving in the New World, encountered these practices and began to integrate them with their own medical traditions brought from their homelands.
During the colonial era, maintaining health was not only a matter of personal well-being but also crucial for the survival and prosperity of the burgeoning communities. Epidemics and severe illnesses posed existential threats, necessitating a community-wide emphasis on health and hygiene. This collective focus laid the groundwork for health to become a core value in American society.
From the implementation of public health measures to prevent the spread of diseases to the establishment of early medical schools, the importance of health was deeply embedded in the fabric of American life. Influential figures, such as Benjamin Franklin and Thomas Jefferson, advocated for public health initiatives, recognizing that a healthy population was vital for the nation’s growth and stability.
As the United States evolved, so did its health priorities. The 19th and 20th centuries saw significant advancements in medical science and public health infrastructure. The establishment of organizations like the American Medical Association and the Centers for Disease Control and Prevention further institutionalized health as a fundamental American value. These developments underscore the historical significance of health in shaping American culture and policies.
Thus, the historical importance of health in American culture is undeniable. It has been a central focus since the early days of the American colonies, influenced by Native American practices and European settlers’ concerns. This enduring emphasis on health has paved the way for the evolution of health priorities in the United States, reflecting a longstanding commitment to the well-being of its citizens.
Health in Colonial America
The health practices and beliefs in colonial America were a blend of traditional remedies, indigenous knowledge, and European medical practices. During this era, healthcare was primarily managed within the household, with a significant role played by midwives and herbalists. Midwives were not only responsible for assisting in childbirth but also acted as general healthcare providers, offering treatments for a variety of ailments using natural remedies derived from plants and herbs.
European medical practices brought to the colonies included the use of bleeding, purging, and other methods based on the humoral theory, which posited that health was maintained by balancing bodily fluids. This theory influenced the treatments administered by colonial physicians, who often combined these methods with local traditions. Additionally, the concept of “materia medica,” a compendium of medicinal substances, was widely utilized, incorporating both European and indigenous knowledge.
Epidemics were a significant challenge in colonial America, with smallpox being one of the most devastating. The impact of smallpox was profound, often decimating entire communities. To combat such epidemics, early public health measures were implemented. One notable method was variolation, an early form of inoculation, where material from a smallpox sore was introduced into a healthy person to induce a mild infection, thereby providing immunity. This practice laid the groundwork for modern vaccination techniques.
Public health initiatives in colonial America also included quarantine measures and the establishment of pest houses to isolate and treat those afflicted with contagious diseases. These early efforts reflected an evolving understanding of disease transmission and the need for communal responses to health crises.
Overall, the health practices in colonial America were a testament to the blend of traditional and European medical knowledge, the crucial role of midwives, and the early public health strategies that aimed to mitigate the impact of epidemics on the burgeoning colonies.
The 19th Century: Industrialization and Health Reforms
The 19th century marked a pivotal era in American public health, significantly influenced by the sweeping changes brought about by industrialization. The rapid growth of urban centers and the rise of factories led to overcrowded living conditions, inadequate sanitation, and a plethora of health issues. These challenges necessitated the development of public health institutions and the implementation of health reforms to mitigate the adverse effects of industrialization on the population.
One of the most notable advancements during this period was the establishment of public health institutions. The first Board of Health in the United States was created in Boston in 1799, but it was not until the 19th century that such institutions became more widespread. These boards played a crucial role in addressing public health concerns, such as sanitation, infectious diseases, and food safety. Their efforts laid the groundwork for modern public health systems and policies that continue to benefit society today.
Simultaneously, the 19th century witnessed the rise of hospitals, transforming them into essential components of the healthcare system. Previously, hospitals were primarily places for the poor and the destitute. However, the increasing understanding of disease and the importance of medical care led to the establishment of more hospitals and improvements in their standards. These institutions began to focus on providing better care, hygiene, and specialized treatments, eventually becoming the centers of medical excellence that we recognize today.
Significant health reforms during this century were championed by key figures, with Florence Nightingale being one of the most influential. Although not American, Nightingale’s contributions had a profound impact on American health practices. Her pioneering work in nursing during the Crimean War and her subsequent efforts in establishing nursing education programs revolutionized healthcare. Nightingale’s emphasis on sanitation, hygiene, and the holistic care of patients inspired numerous reforms in American hospitals and public health policies.
In summary, the 19th century was a transformative period for public health in the United States. The challenges of industrialization spurred the development of public health institutions, the rise of hospitals, and significant health reforms. The contributions of key figures, such as Florence Nightingale, played a crucial role in shaping the American healthcare landscape, laying the foundation for the advancements that followed in the 20th century and beyond.
The 20th Century: Advancements in Medicine and Public Health
The 20th century was a period of remarkable advancements in medicine and public health, which profoundly transformed healthcare in the United States. One of the most significant developments was the creation of vaccines, which played a pivotal role in combating infectious diseases. The introduction of vaccines for polio, measles, mumps, and rubella, among others, led to a dramatic decline in morbidity and mortality rates associated with these illnesses, rendering them largely preventable.
Another landmark in this era was the establishment of the Centers for Disease Control and Prevention (CDC) in 1946. Originally founded to control malaria, the CDC expanded its mission to include the prevention and control of a wide range of infectious diseases, environmental health issues, and chronic diseases. This institution has been instrumental in public health surveillance and outbreak response, solidifying its role as a cornerstone of national and global health security.
The impact of World War I and II on health practices was also profound. The wars necessitated rapid advancements in medical technologies and practices, including the development of antibiotics like penicillin, which revolutionized the treatment of bacterial infections. The exigencies of wartime also led to improvements in surgical techniques, trauma care, and the establishment of blood transfusion services, which have had lasting impacts on civilian healthcare systems.
The rise of health insurance during the 20th century marked another significant shift in American healthcare. Employer-sponsored health insurance became more prevalent, particularly after World War II, as companies began offering health benefits to attract workers. The introduction of Medicare and Medicaid in 1965 under President Lyndon B. Johnson’s administration further expanded access to healthcare. Medicare provided health insurance for Americans aged 65 and older, while Medicaid offered coverage to low-income individuals and families, reducing financial barriers to accessing medical care and improving health outcomes for vulnerable populations.
These advancements and initiatives collectively contributed to a significant improvement in public health and the overall quality of healthcare, setting the stage for continued progress in the 21st century.“`html
Health Movements and Awareness Campaigns
Throughout American history, health movements and awareness campaigns have played pivotal roles in shaping public perception and policy. The anti-smoking campaign, starting in the mid-20th century, marked a significant shift in public health. Spearheaded by the Surgeon General’s 1964 report, it highlighted the severe health risks associated with smoking. Advocacy groups, such as the American Cancer Society and the American Lung Association, championed this cause, leading to widespread public awareness and subsequent legislation. This movement drastically reduced smoking rates and reshaped societal norms around tobacco use.
The fitness craze of the 1980s further underscored the importance of health awareness. This period saw a surge in physical activity, driven by the popularity of aerobics, jogging, and home workout videos. Public figures, such as Jane Fonda, and campaigns like the President’s Council on Physical Fitness and Sports, played crucial roles in promoting an active lifestyle. The fitness movement not only encouraged individuals to incorporate regular exercise into their routines but also laid the groundwork for modern fitness culture, emphasizing the benefits of physical health.
The ongoing battle against obesity represents a more recent and complex health challenge. With obesity rates climbing to alarming levels, public health campaigns have intensified their efforts to address this epidemic. Initiatives such as Michelle Obama’s “Let’s Move!” campaign focused on promoting healthier eating habits and increased physical activity among children. Advocacy groups, including the Obesity Action Coalition, continue to work tirelessly to raise awareness, influence policy, and provide resources to combat obesity. These efforts highlight the multifaceted approach needed to tackle such a pervasive issue effectively.
Advocacy groups have consistently been at the forefront of promoting health issues, often driving significant change. By raising awareness, lobbying for policy changes, and providing education and resources, these organizations have been instrumental in advancing public health initiatives. Whether through grassroots movements or large-scale campaigns, the collective efforts of these groups underscore the ongoing commitment to improving health outcomes for all Americans.
The Role of Technology in Modern Health
Over the past few decades, technology has revolutionized the healthcare sector, introducing innovations that have significantly enhanced patient care and operational efficiency. One of the most notable advancements is telemedicine. This technology allows healthcare providers to consult with patients remotely, thereby improving access to medical care, especially in rural and underserved areas. Telemedicine not only reduces the need for travel, but also minimizes the risk of exposure to infectious diseases, a benefit underscored during the COVID-19 pandemic.
Another critical technological advancement is the implementation of electronic health records (EHRs). EHRs streamline the management of patient information, facilitating better coordination among healthcare providers. This digital transformation reduces paperwork, minimizes errors, and ensures that vital patient information is readily available when needed. EHRs also support data analytics, which can be used to improve patient outcomes and optimize healthcare delivery.
Wearable health technology is another significant contributor to modern health management. Devices such as fitness trackers and smartwatches enable individuals to monitor their health metrics, including heart rate, physical activity, and sleep patterns. These devices promote proactive health management by providing users with real-time data that can be shared with healthcare providers for more personalized care. Additionally, wearables can detect early signs of potential health issues, allowing for timely interventions.
The internet has also played a transformative role in health information dissemination. Patients now have unprecedented access to medical knowledge, empowering them to make informed decisions about their health. Online platforms and mobile applications provide a wealth of information on symptoms, treatments, and preventive measures. However, it is crucial for individuals to rely on reputable sources to avoid misinformation.
In conclusion, the integration of technology in healthcare has led to substantial improvements in patient care and health outcomes. From telemedicine and electronic health records to wearable health tech and the vast resources available online, these advancements have collectively enhanced the efficiency, accessibility, and quality of healthcare services.
Current Health Challenges in America
America today faces a myriad of health challenges that significantly impact its population’s well-being. One of the most pressing issues is the opioid crisis. Over the past decade, opioid addiction has escalated into an epidemic, devastating communities and overwhelming healthcare systems. The misuse of prescription painkillers, heroin, and synthetic opioids such as fentanyl has led to a sharp increase in overdose deaths. Efforts to combat this crisis include stricter prescription regulations, the promotion of alternative pain management therapies, and enhanced addiction treatment programs.
Mental health issues also present a substantial challenge. Conditions such as depression, anxiety, and bipolar disorder affect millions of Americans, yet stigma and inadequate access to mental health care persist. The healthcare system struggles to meet the demand for mental health services, resulting in many individuals not receiving the support they need. Initiatives to improve mental health care include increasing funding for mental health programs, integrating mental health services into primary care, and promoting mental health awareness and education.
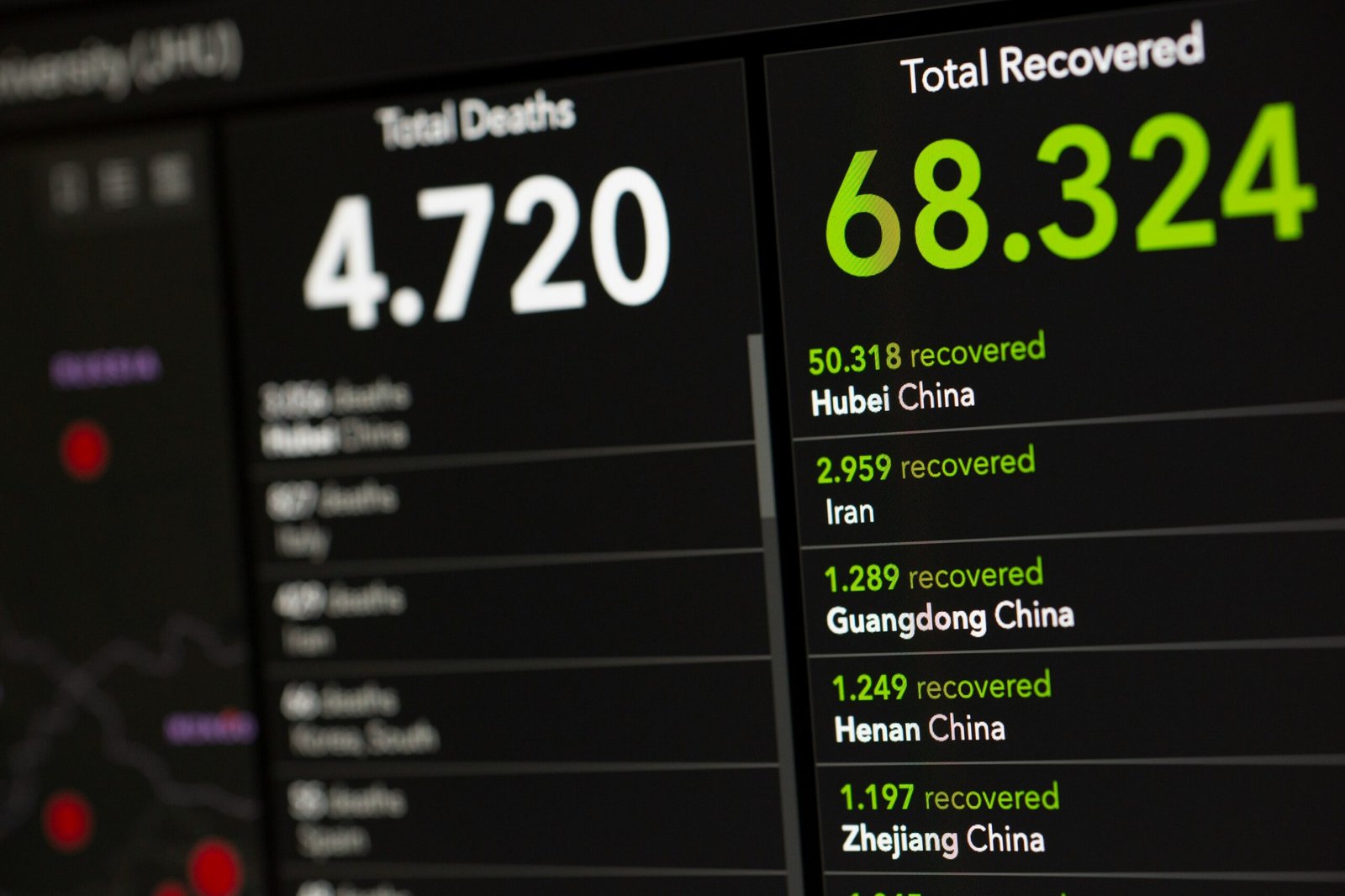
The impact of the COVID-19 pandemic has further exacerbated existing health challenges and introduced new ones. The virus has strained healthcare resources, disrupted routine medical care, and intensified mental health issues due to isolation and economic stress. Efforts to mitigate the pandemic’s impact include widespread vaccination campaigns, public health measures such as mask mandates and social distancing, and ongoing research into effective treatments.
Furthermore, there are significant disparities in healthcare access across different populations. Socioeconomic factors, geographic location, race, and ethnicity can all influence an individual’s ability to obtain quality healthcare. This disparity is evident in higher rates of chronic diseases and lower life expectancy among marginalized communities. Addressing these disparities requires comprehensive strategies, including expanding healthcare coverage, improving healthcare infrastructure in underserved areas, and addressing social determinants of health.
Ongoing efforts to tackle these health challenges involve collaboration among government agencies, healthcare providers, and community organizations. By focusing on prevention, education, and equitable access to care, America can work towards a healthier future for all its citizens.
The Future of Health in America
The future of health in America is poised for transformative advancements, driven by emerging trends in personalized medicine, biotechnology, and artificial intelligence (AI). Personalized medicine, which tailors treatment plans based on individual genetic profiles, is expected to revolutionize patient care. This approach enables more accurate diagnoses, effective treatments, and reduced side effects, marking a significant shift from the traditional one-size-fits-all model.
Biotechnology continues to break new ground in the development of innovative therapies and medical devices. With the advent of CRISPR and other gene-editing technologies, scientists are making strides in treating genetic disorders at their root cause. Furthermore, advancements in biomanufacturing are enhancing the production of complex biological products, from vaccines to regenerative tissue, promising to improve health outcomes significantly.
Artificial intelligence is another critical driver of future healthcare improvements. AI algorithms are increasingly being used to analyze vast datasets, uncovering patterns that can predict and prevent diseases. From AI-powered diagnostic tools that can identify medical conditions with high accuracy to machine learning models that optimize treatment plans, the integration of AI in healthcare is set to improve efficiency, accuracy, and patient outcomes.
Policy changes will also play a pivotal role in shaping the future of health in America. Healthcare reform efforts aimed at expanding access, reducing costs, and improving quality are essential. Policies that promote the adoption of new technologies, support research and development, and encourage preventive care will be crucial in ensuring that advancements in health care are both sustainable and equitable.
Finally, continued public health initiatives remain vital. Efforts to address social determinants of health, enhance health literacy, and promote healthy lifestyles are crucial to improving overall public health. By investing in preventive measures and fostering a culture of wellness, America can create a healthier, more resilient population.
Overview of Key Health Statistics
The health landscape in the United States is shaped by a diverse array of statistics that reflect both progress and ongoing challenges. Below, we present a comprehensive overview of key health indicators, offering insights into life expectancy, leading causes of death, prevalence of chronic diseases, and other critical health metrics.
| Indicator | Value | Notes |
|---|---|---|
| Life Expectancy | 77.3 years | Decreased from 78.8 years in 2019 |
| Leading Cause of Death | Heart Disease | Responsible for 696,962 deaths annually |
| Second Leading Cause of Death | Cancer | Responsible for 602,350 deaths annually |
| Chronic Disease Prevalence | 60% | Adults with at least one chronic condition |
| Obesity Prevalence | 42.4% | Adults aged 20 and over |
These statistics reveal several significant trends. Notably, life expectancy has seen a decline, dropping from 78.8 years in 2019 to 77.3 years in 2023. This decrease can be attributed to a variety of factors, including the impact of the COVID-19 pandemic and rising levels of chronic diseases.
Heart disease remains the leading cause of death, followed closely by cancer. Together, these two conditions account for a substantial number of fatalities each year, underscoring the need for continued research and preventive measures in these areas.
Chronic diseases affect a significant portion of the population, with 60% of adults living with at least one chronic condition. This high prevalence highlights the importance of public health initiatives aimed at managing and preventing chronic illnesses.
Additionally, the prevalence of obesity in adults has reached 42.4%, indicating a critical need for effective interventions to address this issue. Obesity is a major risk factor for a range of health problems, including heart disease, diabetes, and certain cancers.
Overall, these key health statistics provide a snapshot of the current health status in the United States, offering valuable insights into the areas where improvements are needed to enhance the well-being of the population.
Health Disparities and Socioeconomic Factors
Health disparities in the United States are significant and multifaceted, influenced by a range of socioeconomic factors. These disparities manifest across various populations, markedly influenced by income, education, and access to healthcare. For instance, individuals from lower-income backgrounds often face higher rates of chronic diseases and lower life expectancy compared to their wealthier counterparts. This can be attributed to limited access to nutritious food, safe housing, and quality healthcare services.
Moreover, educational attainment is a critical determinant of health. Higher levels of education often correlate with better health outcomes, as education typically provides the necessary skills and knowledge to make informed health decisions, access better employment opportunities, and achieve higher income. Conversely, those with lower educational levels may find themselves in precarious job situations with limited access to employer-provided health benefits, further exacerbating health inequalities.
Geographic location also plays a pivotal role in health outcomes. Rural areas, for instance, often lack adequate healthcare facilities and professionals, leading to delayed diagnoses and treatments. Urban areas, while generally having better access to healthcare, can still exhibit disparities within different neighborhoods, often divided along racial and economic lines.
Below is a table highlighting key differences in health outcomes based on demographics:
| Demographic | Health Outcome | Disparity |
|---|---|---|
| Income Level | Life Expectancy | Low-income individuals have a life expectancy up to 10 years shorter than high-income individuals. |
| Education Level | Chronic Disease Prevalence | Individuals with less than a high school education are twice as likely to suffer from chronic diseases compared to those with a college degree. |
| Geographic Location | Access to Healthcare | Residents of rural areas are 20% more likely to experience inadequate access to healthcare facilities. |
The underlying causes of these disparities are complex and interwoven. Systemic racism, for example, continues to affect the health of racial and ethnic minorities through mechanisms such as discriminatory practices in housing, education, and employment. Additionally, policies that fail to address the social determinants of health perpetuate these inequalities. Current efforts to mitigate health disparities include policy initiatives aimed at expanding healthcare access, improving educational opportunities, and addressing income inequality. Programs like Medicaid expansion and community health interventions are steps in the right direction, but sustained commitment and comprehensive strategies are essential to bridge these gaps effectively.
